Senza categoria
Oral Microbiota: How Therapy Can Combat Periodontitis and Improve Dental Health
Oral health goes far beyond a bright smile; it is a reflection of overall well-being. Periodontitis, one of the most common gum diseases, can lead to serious consequences if neglected. But did you know that the oral microbiota plays a crucial role in fighting this condition? Recent studies have revealed how targeted therapy can rebalance the microorganisms present in the mouth, improving not only oral health but also overall health status. In this article, we will explore the links between the oral microbiota and periodontitis, discovering how innovative therapeutic strategies can prevent dental deterioration and restore a healthy smile. Get ready to discover how taking care of your mouth can become a fundamental part of the journey toward well-being!
What is the Oral Microbiota?
The oral microbiota is the collection of microorganisms residing in our mouth, including bacteria, fungi, viruses, and protozoa. This complex ecosystem plays a crucial role in maintaining oral health and, consequently, general well-being. Every individual possesses a unique oral microbiota composition, influenced by genetic factors, lifestyle, diet, and oral hygiene. The mouth mainly hosts bacteria (around 700 species), which coexist in a dynamic balance, helping to protect teeth and gums from infections.
The oral microbiota is not static; it evolves and changes in response to various stimuli, such as the consumption of food and drinks, the use of antibiotics, and even stress. This balance can be easily disrupted, leading to pathological conditions such as periodontitis. The presence of beneficial bacteria is essential for preventing the proliferation of harmful microorganisms, which can cause inflammation and damage to oral tissues. A healthy microbiota acts as a natural barrier against infections, but when this barrier is compromised, oral health suffers.
Understanding the oral microbiota is fundamental for developing new targeted therapeutic strategies. With the advancement of DNA sequencing techniques, researchers are able to precisely identify and study the different species present in the oral cavity, paving the way for personalized treatments. These advancements allow us to see oral health in a completely new light, where the prevention and care of gum diseases can be addressed with a holistic approach based on microbiota balance.
Periodontitis: Causes and Symptoms
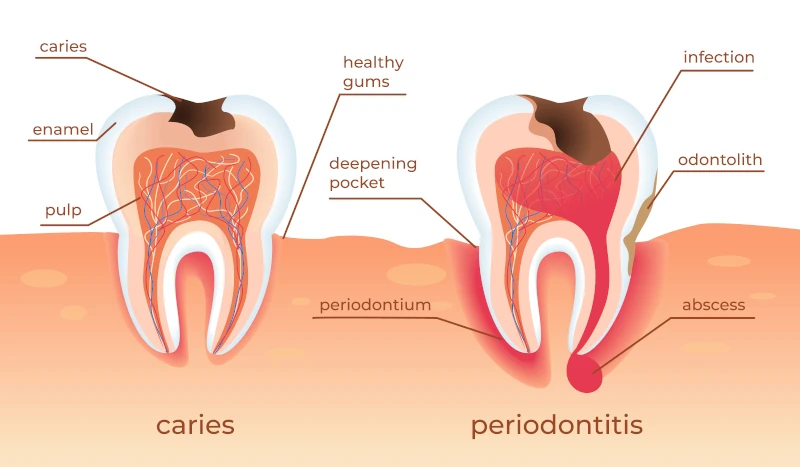
Periodontitis is a chronic inflammatory disease that affects the supporting tissues of the teeth, including the gums, periodontal ligaments, and alveolar bone. It is one of the main causes of tooth loss in adults and represents a serious threat to oral health. The causes of periodontitis are multifactorial, including the presence of pathogenic bacteria, an altered immune response, genetic factors, and unhealthy lifestyle habits such as smoking and a poor diet.
The symptoms of periodontitis can range from mild to severe. In the early stages, it often manifests as gingivitis, characterized by red, swollen, and bleeding gums. If left untreated, the inflammation can progress, leading to the destruction of supporting tissues and the formation of periodontal pockets. These pockets offer an ideal environment for the proliferation of pathogenic bacteria, further aggravating the condition. Other symptoms of advanced periodontitis include tooth mobility, persistent bad breath, pain during chewing, and gum recession.
Early diagnosis of periodontitis is essential to prevent irreversible damage. Regular dental visits and good oral hygiene are fundamental for keeping gum health under control. However, understanding the role of the oral microbiota in periodontitis is opening new possibilities for the prevention and treatment of this condition. Targeted therapies that rebalance the microbiota can offer an innovative and more effective approach to combating periodontitis.
The Importance of the Microbiota in Oral Health
The oral microbiota plays a crucial role in maintaining oral health through various mechanisms. First of all, the beneficial bacteria present in the oral cavity compete with pathogens for resources and space, thereby limiting their proliferation. This phenomenon, known as competitive exclusion, is fundamental for preventing infections and maintaining a healthy oral environment. Furthermore, some microbiota bacteria produce natural antimicrobial substances that inhibit the growth of harmful microorganisms.
A balanced oral microbiota also contributes to the modulation of the immune response. Beneficial microorganisms interact with immune cells present in the gums, stimulating an appropriate response that protects tissues without causing excessive inflammation. This interaction is essential for preventing chronic inflammatory diseases such as periodontitis. Additionally, a healthy microbiota promotes the production of anti-inflammatory substances, further helping to maintain the balance of the oral immune system.
Dysbiosis, which is the alteration of the oral microbiota balance, is associated with various pathological conditions. When the number of pathogenic bacteria exceeds that of beneficial microorganisms, an environment prone to infections and inflammation is created. This imbalance can be caused by various factors, including poor oral hygiene, excessive use of antibiotics, a diet rich in sugars, and smoking. Understanding the importance of the oral microbiota is therefore essential for developing targeted preventive and therapeutic strategies to maintain and restore microbiotic balance.
How Microbiota Therapy Can Prevent Periodontitis
Oral microbiota therapy represents an innovative and promising approach for the prevention and treatment of periodontitis. This strategy is based on restoring the microbiota’s natural balance, promoting the proliferation of beneficial bacteria and reducing the presence of pathogens. One of the main techniques used is the application of probiotics, live microorganisms that confer health benefits to the host. Probiotics can be administered through supplements, functional foods, or oral hygiene products such as toothpastes and mouthwashes.
Another effective method is the use of prebiotics, non-digestible substances that stimulate the growth and activity of beneficial bacteria in the oral cavity. Prebiotics can be included in the daily diet through the consumption of fiber-rich foods such as fruits, vegetables, and whole grains. Integrating prebiotics and probiotics into the daily routine can help maintain a healthy oral microbiota, thus preventing the onset of gum diseases.
In addition to probiotics and prebiotics, microbiota therapy can involve the use of selective antibiotics that eliminate specific pathogenic bacteria without harming the beneficial microorganisms. This targeted approach reduces the risk of dysbiosis and minimizes the side effects associated with the indiscriminate use of antibiotics. The integration of these diverse therapeutic strategies offers a powerful means to prevent periodontitis and maintain long-term oral health.
Types of Oral Microbiota Therapies
Various therapies targeting the oral microbiota exist, each with its own mechanism of action and specific application. One of the most common is the use of probiotics, which can be administered through various means such as oral supplements, enriched yogurt, and dental hygiene products. Probiotics such as Lactobacillus and Bifidobacterium are known for their beneficial effects, including the ability to inhibit pathogenic bacteria and reduce gum inflammation.
Another effective therapy is the use of prebiotics, substances that feed the beneficial bacteria already present in the microbiota. Prebiotics include dietary fibers such as inulin and fructo-oligosaccharides, which can be found in foods like chicory, garlic, and bananas. Including these foods in the daily diet helps promote a healthy oral environment and prevent the proliferation of harmful bacteria.
Selective antibiotic therapies represent a more advanced solution, aimed at specifically eliminating pathogenic bacteria without destroying the beneficial microbiota. This approach requires precise diagnosis and identification of the pathogenic microorganisms present in the oral cavity. Antibiotics can be administered locally in the form of gels or mouthwashes, thus reducing the risk of systemic side effects. These targeted antibiotic therapies are particularly useful in cases of advanced periodontitis, where a more aggressive intervention is necessary to restore oral health.

Diet and Microbiota: Foods that Promote Dental Health
Diet plays a fundamental role in maintaining a healthy oral microbiota and preventing gum diseases. A balanced, nutrient-rich diet can promote the proliferation of beneficial bacteria and reduce the growth of pathogenic microorganisms. Fiber-rich foods, such as fruits, vegetables, and whole grains, are particularly useful as they act as prebiotics, feeding the good bacteria and promoting a healthy oral environment.
Some foods, such as green tea, contain natural antimicrobial compounds that help fight pathogenic bacteria. Green tea is rich in catechins, antioxidants that have been shown to reduce inflammation and inhibit the growth of bacteria responsible for periodontitis. Dairy products, such as yogurt and cheese, are also beneficial for oral health due to their calcium and phosphate content, which help remineralize teeth and maintain the balance of the microbiota.
The consumption of refined sugars and processed foods should be limited, as these can promote the growth of pathogenic bacteria and increase the risk of cavities and gum diseases. Instead, it is advisable to opt for whole and unrefined foods, which not only support oral health but also improve general well-being. Hydration is equally important: drinking plenty of water helps keep the mouth clean and reduce the accumulation of bacterial plaque.

Probiotics and Prebiotics: Their Role in Oral Health
Probiotics and prebiotics play a crucial role in maintaining a balanced oral microbiota and preventing gum diseases. Probiotics are live microorganisms that, when consumed in adequate amounts, confer health benefits to the host. They can be found in fermented foods such as yogurt, kefir, sauerkraut, and kimchi, as well as in specific supplements. Probiotics act by competing with pathogenic bacteria for resources and space, producing natural antimicrobial substances, and modulating the immune response.
Prebiotics, on the other hand, are non-digestible substances that promote the growth and activity of beneficial bacteria in the oral cavity. They are present in fiber-rich foods such as fruits, vegetables, legumes, and whole grains. Prebiotics stimulate the proliferation of probiotics, creating a favorable environment for a healthy oral microbiota. Integrating probiotics and prebiotics into the daily diet can significantly improve oral health, reducing gum inflammation and preventing periodontitis.
Numerous studies have demonstrated the effectiveness of probiotics and prebiotics in the treatment of gum diseases. For example, the use of specific probiotics such as *Lactobacillus reuteri* has been associated with a significant reduction in bacterial plaque and gum inflammation. Similarly, prebiotic intake has been shown to improve the balance of the oral microbiota and reduce the symptoms of periodontitis. These results highlight the importance of a diet rich in probiotics and prebiotics for maintaining oral health.
Recent Studies on Microbiota Therapy and Periodontitis
In recent years, numerous studies have explored the role of the oral microbiota in periodontitis and the effectiveness of microbiota-targeted therapies in the treatment of this disease. Research has shown that periodontitis is associated with oral microbiota dysbiosis, characterized by an increase in pathogenic bacteria and a reduction in beneficial microorganisms. Studies suggest that restoring the microbiota balance can be an effective strategy for preventing and treating periodontitis.
An important study conducted at the University of Zurich examined the effectiveness of probiotics in the treatment of periodontitis. Researchers administered *Lactobacillus reuteri* supplements to a group of patients with severe periodontitis. The results showed a significant reduction in bacterial plaque and gum inflammation, highlighting the potential of probiotics as a complementary therapy for gum diseases. Another study, published in the *Journal of Clinical Periodontology*, examined the use of prebiotics such as inulin in improving oral microbiota balance and reducing the symptoms of periodontitis.
In addition to probiotics and prebiotics, research is exploring other innovative therapies such as the use of selective antibiotics and gene therapies to modulate the oral microbiota. For example, a study conducted at Harvard University developed a new targeted antibiotic that eliminates specific pathogenic bacteria without harming beneficial microorganisms. These promising results pave the way for new therapeutic strategies for managing periodontitis and maintaining oral health.

Practical Tips for Maintaining a Healthy Oral Microbiota
Maintaining a healthy oral microbiota is essential for preventing gum diseases and promoting general well-being. One of the most important practices is good oral hygiene, which includes brushing your teeth after meals and using dental floss to remove food remnants between your teeth.
Diet plays a crucial role in maintaining the balance of the oral microbiota. It is important to follow a diet rich in fruits, vegetables, whole grains, and fermented foods, which provide natural prebiotics and probiotics. Limiting the intake of refined sugars and processed foods can reduce the risk of cavities and gum diseases, preventing the proliferation of pathogenic bacteria. Drinking plenty of water is equally important for keeping the mouth hydrated and reducing plaque accumulation.
Regular visits to the dentist and oral hygienist are essential for monitoring oral health and identifying any problems early. The dentist can provide personalized advice for maintaining a healthy oral microbiota and recommend specific treatments if necessary. Furthermore, avoiding harmful habits such as smoking and excessive alcohol consumption can significantly contribute to maintaining microbiota balance and preventing gum diseases. Adopting these daily practices can help maintain a healthy mouth and a bright smile.
Conclusion: The Future of Oral Health Through the Microbiota
The oral microbiota is emerging as a key element in the understanding and treatment of gum diseases such as periodontitis. Research continues to reveal new details on how the microorganisms present in the mouth influence oral and general health, paving the way for innovative and personalized therapies. Microbiota therapy, through the use of probiotics, prebiotics, and selective antibiotics, offers a promising approach to prevent and treat periodontitis effectively and sustainably.
The importance of maintaining a balanced oral microbiota cannot be underestimated. Daily practices such as good oral hygiene, a balanced diet, and regular dental visits are fundamental for supporting the health of the microbiota and preventing gum diseases. Furthermore, adopting healthy habits such as avoiding smoking and limiting the consumption of refined sugars can significantly contribute to maintaining a healthy oral environment.
The future of oral health is promising, with more and more studies exploring the role of the microbiota and developing new targeted therapies. Understanding and exploiting the potential of the oral microbiota can transform the way we prevent and treat gum diseases, improving oral health and general well-being. Taking care of the oral microbiota is a fundamental part of the journey toward a healthy and lasting smile.